
Welcome to our comprehensive guide on 12 essential at-home physical therapy techniques for accelerated postoperative rehabilitation.
Designed to empower individuals seeking freedom and independence in their recovery journey, this article provides a knowledgeable and professional insight into various exercises, techniques, and strategies for optimal rehabilitation.
From range of motion exercises to pain management techniques, balance and stability training to cardiovascular conditioning, our expert-recommended methods will help you achieve accelerated postoperative recovery in the comfort of your own home.
Preparing for At-Home Rehabilitation
As we delve into the topic of preparing for at-home rehabilitation, it is important to consider various strategies that can optimize the effectiveness of postoperative recovery.
Pre-operative preparation plays a crucial role in setting the stage for successful rehabilitation at home. This includes educating patients about the importance of adhering to their home exercise program and providing them with a clear understanding of the exercises they need to perform. The design of the home exercise program should be tailored to the individual's specific needs and goals, taking into account their surgical procedure and any restrictions or limitations they may have.
It is essential to provide detailed instructions and demonstrations to ensure proper execution of exercises. Additionally, providing patients with resources such as instructional videos or written guides can further enhance their understanding and compliance with the program.
Range of Motion Exercises
Patients should incorporate range of motion exercises into their home exercise program to improve flexibility and joint mobility. These exercises are crucial for maintaining and increasing the range of motion in joints, which is essential for performing daily activities with ease and reducing the risk of injury.

Here are four flexibility training techniques that can be incorporated into a home exercise program:
Passive range of motion exercises: These exercises involve the therapist or a caregiver moving the patient's joints through their full range of motion. This helps to maintain joint mobility and prevent stiffness.
Active-assistive range of motion exercises: In these exercises, the patient uses their own muscles to move their joints, but with the assistance of a therapist or a device. This helps to gradually increase the joint's range of motion.
Stretching exercises: Stretching is an effective way to improve flexibility. Patients can perform static stretches, where they hold a stretch for a certain period of time, or dynamic stretches, where they move through a range of motion repeatedly.
Joint mobilization techniques: These techniques are performed by a therapist and involve applying gentle pressure to the joint to improve its mobility and reduce pain.
Strengthening Exercises for Targeted Areas
Strengthening exercises for targeted areas are an essential component of postoperative rehabilitation.
Core stability exercises help improve overall strength and stability, while upper body strengthening exercises focus on improving the strength of the arms, shoulders, and chest.

Additionally, lower body workouts target the muscles in the legs and hips, helping to regain mobility and strength.
These exercises, when performed correctly and consistently, can greatly contribute to a successful recovery process.
Core Stability Exercises
Implementing a variety of targeted exercises can significantly enhance core stability, helping to improve overall strength and prevent potential injuries.
Core stability exercises are designed to strengthen the muscles in the abdomen, back, and pelvis, which provide a solid foundation for movement and support for the spine.
The benefits of core stability are numerous and include improved posture, increased balance and stability, reduced risk of back pain, and enhanced athletic performance.
By engaging in regular core stability exercises, individuals can experience greater freedom of movement, increased confidence in their physical abilities, and a decreased likelihood of sustaining injuries during daily activities or sports.
Whether it's through planks, bridges, or rotational movements, incorporating core stability exercises into a fitness routine can have a profound impact on overall well-being and physical freedom.

Upper Body Strengthening
In order to optimize their postoperative rehabilitation, individuals may benefit from incorporating upper body strengthening exercises, such as push-ups or dumbbell curls, into their at-home PT routine. These exercises specifically target the shoulders and arms, helping to improve muscle strength, endurance, and flexibility.
Shoulder exercises, such as shoulder presses or lateral raises, can help strengthen the deltoid muscles, which are crucial for shoulder stability and mobility. Additionally, arm strengthening exercises like bicep curls or tricep extensions can enhance the strength and stability of the arm muscles, aiding in everyday activities such as lifting and carrying objects.
Lower Body Workouts
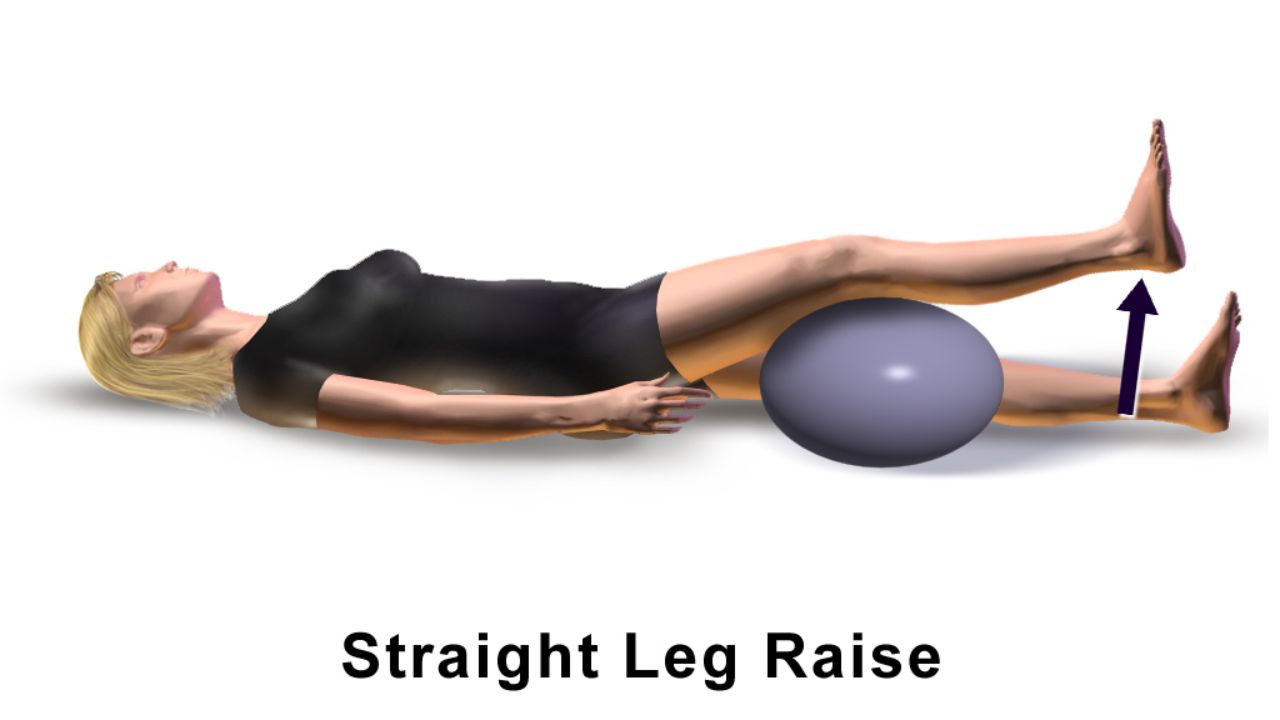
Three effective lower body workouts can help improve muscle strength, stability, and mobility in targeted areas such as the hips, thighs, and calves. These workouts are not only beneficial for athletes or fitness enthusiasts but also for individuals seeking functional rehabilitation and injury prevention. Incorporating these exercises into your routine can enhance lower body performance and reduce the risk of future injuries.
Here are four essential lower body workouts to consider:
Squats: Squats engage multiple muscle groups, including the quadriceps, hamstrings, glutes, and calves, promoting overall lower body strength and stability.
Lunges: Lunges target the muscles of the thighs and hips, promoting balance and stability while also improving flexibility and range of motion.
Deadlifts: Deadlifts primarily target the hamstrings, glutes, and lower back muscles, helping to build strength and stability in the posterior chain.

Calf raises: Calf raises focus on the calf muscles, improving ankle strength and stability, which is essential for activities such as running and jumping.
Balance and Stability Training
Exercising proprioceptive control through targeted balance and stability training enhances postoperative recovery and reduces the risk of future injuries. Balance training and stability exercises are essential components of rehabilitation programs designed to optimize functional outcomes after surgery. These exercises focus on improving coordination, strength, and control of the body's movements, ultimately enhancing overall stability and reducing the risk of falls or further injuries.
Balance training involves challenging the body's ability to maintain equilibrium in various positions and situations. This can include exercises such as single-leg stands, heel-to-toe walking, and balancing on unstable surfaces. Stability exercises, on the other hand, focus on strengthening the muscles that support the joints and spine, improving overall stability and control.
By incorporating these exercises into postoperative rehabilitation programs, patients can improve their ability to move safely and confidently, regain functional independence, and prevent future injuries. These exercises are particularly beneficial for individuals recovering from orthopedic surgeries or those with conditions that affect balance and stability, such as ankle sprains or knee injuries.
Pain Management Techniques
Effective pain management techniques are crucial for optimizing patient comfort and facilitating the recovery process after surgery or injury. Here are four key techniques that can greatly assist in pain management:
Medication: The use of appropriate pain medications, such as opioids or nonsteroidal anti-inflammatory drugs (NSAIDs), can provide relief and improve overall comfort.
Physical therapy: Engaging in specific exercises and stretches prescribed by a physical therapist can help alleviate pain, improve range of motion, and promote healing.

Scar tissue massage and management: Massaging the area around surgical or injury scars can help break down scar tissue, reduce pain, and improve mobility.
Alternative therapies: Techniques such as acupuncture, chiropractic adjustments, and mindfulness meditation can offer additional pain relief options for those seeking alternatives to traditional medication.
Scar Tissue Massage and Management
Scar tissue massage and management is a crucial aspect of postoperative rehabilitation. It involves applying specific massage techniques to the area of scar tissue to promote healing, improve flexibility, and reduce pain.
This form of therapy has been proven to be effective in breaking down scar tissue and restoring normal function, making it an essential component of recovery.
Massage Techniques Explained
During the therapeutic process, proper massage techniques can assist in the management and reduction of scar tissue formation. Scar tissue can be a result of various factors, such as surgery, injury, or repetitive strain. Massage therapy can help break down the dense collagen fibers that make up scar tissue, improving its flexibility and reducing its appearance.
Here are four essential massage techniques for scar tissue management:
Effleurage: Gentle, sweeping strokes that promote lymphatic drainage and increase blood flow to the scar area.

Friction: Deep, circular motions that target the scar tissue directly, breaking down adhesions and promoting collagen remodeling.
Petrissage: Kneading and lifting motions that help stretch and loosen the scar tissue, improving its pliability.
Myofascial release: Applying sustained pressure to the surrounding muscles and fascia to release tension and improve scar tissue mobility.
Benefits of Scar Massage
Regular scar massage, along with other postoperative rehabilitation techniques, can contribute to improved tissue healing and reduced scar formation. Scar tissue mobilization is a key component of scar management, as it helps break down adhesions and improve the flexibility of the scar tissue.
This technique involves applying pressure and gently massaging the scar using specific strokes and techniques. Scar tissue management techniques also include stretching exercises, application of silicone gel sheets, and use of topical creams or ointments. These interventions aim to minimize scar tissue formation, improve scar appearance, and enhance overall tissue healing.
Benefits of scar tissue mobilization include increased blood flow to the area, improved range of motion, reduction in scar tightness, and decreased pain or discomfort. It is important to consult with a healthcare professional or physical therapist for guidance on proper scar management techniques.
Neuromuscular Reeducation Exercises
One must diligently incorporate neuromuscular reeducation exercises into their postoperative rehabilitation routine to optimize functional recovery and restore proper muscle activation patterns. These exercises, which focus on improving the communication between the nerves and muscles, play a crucial role in regaining strength, coordination, and balance after surgery.
Here are four key benefits of incorporating neuromuscular reeducation techniques and proprioceptive exercises into your rehabilitation routine:
Enhanced muscle activation: These exercises help activate specific muscles or muscle groups, ensuring they are firing correctly and efficiently.
Improved coordination and balance: By targeting the neuromuscular pathways, these exercises help improve coordination and balance, reducing the risk of falls and enhancing overall mobility.
Restored functional movement patterns: Neuromuscular reeducation techniques help retrain the muscles to perform their intended actions, leading to restored functional movement patterns.
Increased proprioception: Proprioceptive exercises enhance the body's ability to sense joint position and movement, allowing for better control and stability during activities.
Joint Mobilization Techniques
Joint mobilization techniques are a key component of physical therapy, aimed at improving joint range of motion and reducing pain. These techniques involve skilled manual therapy interventions, such as passive oscillatory movements, sustained stretching, or manipulation, to address joint restrictions and restore normal joint function.
However, it is crucial to consider safety considerations, such as assessing patient tolerance, monitoring for adverse effects, and ensuring proper technique application, to optimize the benefits and minimize potential risks associated with joint mobilization.

Benefits of Mobilization
The therapist's expertise in mobilization techniques can greatly enhance the patient's recovery and overall rehabilitation process. Here are four key benefits of mobilization:
Improved Joint Flexibility: Mobilization techniques help to increase the range of motion in joints, allowing for better movement and function. This can be particularly beneficial for individuals recovering from surgery or injury.
Pain Reduction: Mobilization techniques, such as joint mobilizations and soft tissue mobilizations, can help to alleviate pain by reducing inflammation and promoting blood flow to the affected area.
Enhanced Healing: By promoting blood flow and stimulating the healing process, mobilization techniques can help to speed up recovery time and improve overall healing outcomes.
Increased Independence: By improving joint flexibility and reducing pain, mobilization techniques can empower patients to regain their independence and engage in activities they may have previously been unable to do.
Safety Considerations for Mobilization
Several important safety considerations must be taken into account when implementing mobilization techniques for joint rehabilitation. Precautions must be followed to ensure the well-being of the patient and to prevent any potential risks or injuries.
First and foremost, it is crucial to assess the patient's condition and suitability for mobilization techniques. This involves considering factors such as the severity of the injury, the presence of any underlying medical conditions, and the patient's overall physical health.

Additionally, proper technique is paramount in ensuring safe and effective mobilization. Healthcare professionals should be well-trained in the specific mobilization techniques and should adhere to proper body mechanics and positioning. This includes maintaining a stable base of support, using appropriate hand placement, and applying gradual and controlled forces during mobilization.
Postural Correction and Alignment Exercises
While engaging in postural correction and alignment exercises, individuals should focus on maintaining proper form throughout each movement to optimize their rehabilitation progress. Proper form is crucial in order to target the correct muscles and prevent any further injury or strain. Here are four essential tips to ensure correct form and maximize the benefits of postural correction techniques and alignment exercises:
Mindful awareness: Stay present and focus on the alignment of your body during each exercise. Pay attention to your posture, spinal alignment, and the engagement of the targeted muscles.
Gradual progression: Start with gentle exercises and gradually increase the intensity and duration. This allows your body to adapt and prevent any unnecessary strain.
Breath control: Coordinate your breath with each movement. Inhale deeply before starting the exercise and exhale as you perform the movement. This helps stabilize your core and improve overall control.
Regular practice: Consistency is key. Aim to incorporate postural correction and alignment exercises into your daily routine to see long-term improvements in your posture and alignment.
Cardiovascular Conditioning
One can enhance their cardiovascular conditioning by incorporating regular aerobic exercises into their fitness regimen. Cardiovascular endurance, also known as aerobic conditioning, is an essential component of overall fitness and health. It refers to the ability of the heart, lungs, and blood vessels to deliver oxygen and nutrients to the muscles during prolonged physical activity.

Regular aerobic exercise helps improve cardiovascular endurance by strengthening the heart and lungs, increasing the efficiency of oxygen transport, and improving the body's ability to use oxygen during exercise. Some popular aerobic exercises include running, cycling, swimming, and brisk walking. These activities elevate the heart rate and keep it elevated for an extended period, challenging the cardiovascular system and leading to improvements in cardiovascular endurance over time.
Incorporating regular aerobic exercise into one's fitness routine can provide numerous health benefits, such as reducing the risk of heart disease, improving lung function, and increasing energy levels.
Functional Training for Daily Activities
In order to improve functional fitness and enhance one's ability to perform daily activities, it is important to incorporate functional training exercises that mimic real-life movements into a regular exercise routine. Functional training focuses on strengthening the muscles and movements that are necessary for everyday tasks, such as bending, lifting, and reaching.
For older adults, functional training is especially beneficial as it helps maintain independence and promotes a higher quality of life. To support functional training for older adults, adaptive equipment for daily activities can be used to assist with mobility and enhance stability. This includes items such as grab bars, walking aids, and modified kitchen utensils.
Progress Tracking and Goal Setting
When implementing a comprehensive exercise program, progress tracking and goal setting are essential for ensuring consistent improvement and optimizing results.
Progress tracking allows individuals to monitor their performance and identify areas for improvement. It provides valuable feedback on the effectiveness of the exercise program and helps individuals stay motivated by seeing their progress over time.
Goal setting, on the other hand, provides a clear target to work towards and helps individuals stay focused and committed to their exercise routine. By setting specific, measurable, attainable, relevant, and time-bound goals, individuals can effectively track their progress and make adjustments to their program as needed.

Whether it's increasing strength, improving cardiovascular endurance, or losing weight, progress tracking and goal setting are vital tools to achieve desired outcomes and maintain a sense of freedom in one's fitness journey.
Frequently Asked Questions
How Long Does the Postoperative Rehabilitation Process Typically Last?
The duration of postoperative rehabilitation varies depending on several factors such as the type of surgery, individual patient characteristics, and adherence to therapy. It is important to follow a personalized rehabilitation plan to achieve accelerated recovery.
Are There Any Specific Dietary Guidelines or Restrictions to Follow During At-Home Rehabilitation?
Dietary guidelines and nutritional recommendations play an important role in at-home rehabilitation postoperatively. Following specific dietary guidelines and restrictions can aid in the healing process and promote accelerated recovery.
How Can I Manage Swelling and Inflammation During the Recovery Process?
Swelling management and inflammation control are crucial aspects of the recovery process. Various techniques such as elevation, cold therapy, compression, and anti-inflammatory medications can be used to effectively manage swelling and reduce inflammation.
Are There Any Precautions or Modifications Needed for Individuals With Pre-Existing Medical Conditions During At-Home Rehabilitation?
Precautions and modifications are necessary for individuals with pre-existing medical conditions during at-home rehabilitation. It is important to tailor the rehabilitation program to accommodate their specific needs and minimize any potential risks or complications.
Are There Any Recommended Assistive Devices or Equipment That Can Aid in the Rehabilitation Process at Home?
Assistive devices and recommended equipment can greatly aid in the rehabilitation process at home. These tools provide support, stability, and assistance in performing exercises and activities, ensuring a safe and effective recovery.
Conclusion
In conclusion, implementing at-home physical therapy techniques can greatly accelerate postoperative rehabilitation.

By focusing on range of motion exercises, strengthening targeted areas, balance and stability training, pain management techniques, postural correction and alignment exercises, cardiovascular conditioning, functional training for daily activities, and progress tracking and goal setting, individuals can optimize their recovery process.
By following these essential techniques, patients can improve their overall physical function and regain independence more quickly.
 Mobility trainingHome Fitness RecoverySports Injury PreventionPersonal Physical TherapyOrthopedic SolutionsPrivacy PolicyTerms And Conditions
Mobility trainingHome Fitness RecoverySports Injury PreventionPersonal Physical TherapyOrthopedic SolutionsPrivacy PolicyTerms And Conditions
